It can be a shock if your child is diagnosed with type 1 diabetes, but with an estimated 6500 Australian children aged 0–14 affected, you are certainly not alone.
Diabetes is one of the most common chronic childhood conditions. It can be overwhelming, confusing and worrying as you, your child and other members of the family adapt to such a life-changing diagnosis.
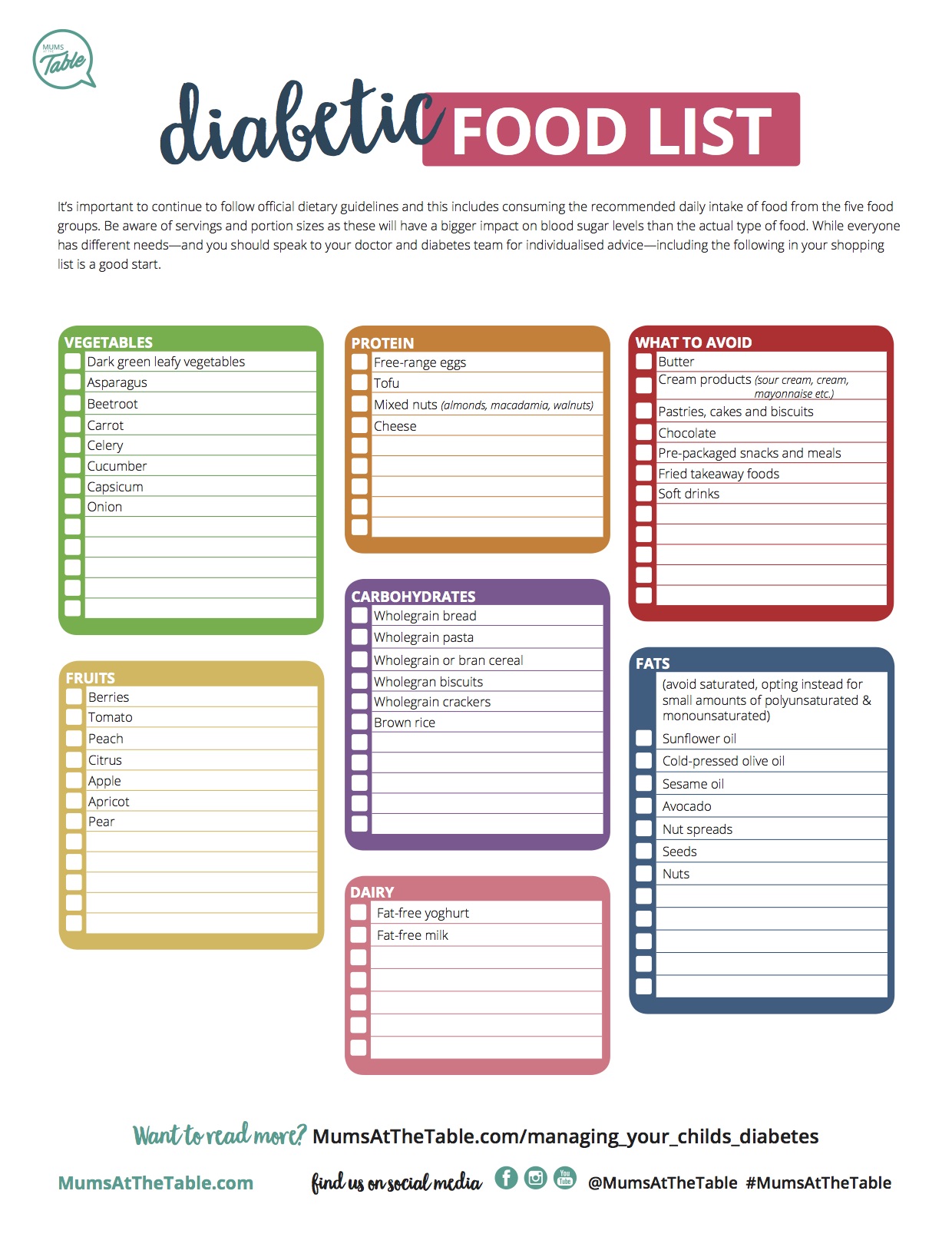
This article will focus on type 1 diabetes, which is more commonly diagnosed in young people. We’ll tell you the risk factors and symptoms of the disease, as well as how to manage it, if your child has been diagnosed. Read on to the end for a free diabetic food list printable, to help your child maintain a healthy diet, giving them the best chance to fight the disease.
The difference between type 1 and type 2 diabetes
Type 1 diabetes is an autoimmune disease in which the body’s immune system is activated to destroy the cells in the pancreas that produce insulin. It is not due to lifestyle factors and cannot be prevented or cured.
When the body doesn’t produce enough insulin, it leads to high blood sugar levels (glucose). This can lead to both short-term health problems and long-term complications if not well managed. People with type 1 diabetes need insulin every day to keep them alive.
Without insulin, the body burns its own fat, which produces ketones. This can lead to a dangerous condition called diabetic ketoacidosis (DKA). Fruity-smelling breath is often a sign of having high levels of ketones.
In children, type 2 diabetes is much less common than type 1 diabetes. Children with an unhealthy lifestyle, poor diet, lack of exercise, obesity and sometimes genetic factors, are at an increased risk of developing type 2 diabetes. There are only approximately 400 cases diagnosed each year amongst 10- to 24-year-olds.
Symptoms of type 1 diabetes
It’s always better to be on the safe side when it comes to type 1 diabetes. Testing is advisable if your child suddenly displays these symptoms:
- Excessive thirst
- Asking to go to the toilet more frequently
- Bedwetting, when they have previously been consistently dry at night
- Lethargic or increased feelings of tiredness
- Unexplained sudden weight loss
- Blurred vision
- Skin infections or cuts that heal slowly
The diagnosis of diabetes is a relatively simple process. A visit to the GP to explain your child’s symptoms should lead to a finger-prick blood test in the office and a venous blood glucose test if the doctor has concerns.
If your child is diagnosed with type 1 diabetes, it is important to remember there is plenty of support to help manage it and to allow your child to live a healthy and happy life. Young children with newly-diagnosed diabetes are often admitted to hospital for a few days where there is lots of medical advice and support available from diabetes nurse educators, doctors, dietitians and sometimes, psychologists. Looking after a child with type 1 diabetes is best done by an experienced multidisciplinary team.
Your child should be involved in as much of the conversation as possible between you and their doctor to increase their understanding of type 1 diabetes. This will help with everyday diabetes care and management, and enable them to become independent and take more responsibility as they transition to the teenage and young adult years.
Treatment and management of type 1 diabetes
Your child will need to monitor their blood glucose level up to six times per day. An alternative is continuous glucose monitoring or CGM, which is now government-funded for Australians under the age of 21 who have type 1 diabetes.
Insulin is given by multiple daily injections into the skin or via an insulin pump. Keeping blood glucose levels in the optimum range is a careful balance between what food is eaten, the dosage given for insulin injections and physical activity levels.
Read: “Please, no more needles,” he pleaded while hiding under the table
Insulin pumps are similar in size to a mobile phone, battery operated and hold a small amount of insulin. Worn 24 hours a day under a child’s shirt or dress, a pump is programmed to deliver insulin into the body through a small plastic tube, enabling a more flexible lifestyle compared to injections, and allowing your child to have better control over their diabetes. Children with pumps can still play sport and in fact may have more stable glucose levels after exercise than children on multiple daily injections.
Heart-healthy diets that are low in cholesterol and saturated fats will not only benefit your diabetic child, but the entire family as well. (Scroll to the end for our free diabetic food list printable.)
Having diabetes can be both a physical and psychological battle at times. In the early days, it’s not unusual for your child to feel down and isolated or despise the effort that management of their diabetes requires.
Seeing a diabetes educator, psychologist, social worker or endocrinologist may help with this, as will the establishment of a diabetes management plan. It is helpful to ensure that your child’s school is fully informed and becomes a partner in the monitoring and management plan.
There will come a point in your child’s life between the ages of 16 and 18 when they will make the move from medical support services specific to childhood to adult medical care. While this can be daunting for you and your child, your health care professionals are experienced to help with this transition.
If your child develops type 1 diabetes, they will need regular monitoring and good management to stay healthy, but diabetes will not stop them from enjoying a happy and very active life.
A note about hypoglycemia

A hypoglycemic episode or “hypo” is a low blood glucose level (below 4mmol/L) causing hunger, sweating, trembling, paleness, dizziness, headache and sometimes confusion or irritability.
Hypoglycemia can be caused by too much insulin, delaying or missing a meal, not eating enough carbohydrates, unplanned physical activity or alcohol consumption. It is treated with high sugar food or drinks such as jelly beans or orange juice initially, followed by a longer-acting carbohydrate food such as a slice of bread.
Free diabetic food list printable
While everyone has different needs—and you should speak to your doctor and diabetes team for individualised medical advice—including the following in your shopping list is a good start.

How helpful was this article?
Click on a star to rate it!
5 / 5. 1
Be the first to rate this post!
Dr Katherine Benson
Related posts
Subscribe
Receive personalised articles from experts and wellness inspiration weekly!


